Risk is the impact of uncertainty on achieving your objectives – the impact can be either positive or negative outcomes (ISO 31000). Governments have multiple objectives they have to meet – health and wellbeing, economic, environmental, ethical and so on. Each of these objectives essentially becomes a risk endpoint. The fundamental tenets of risk assessment are understanding the system (the context), understanding and assessing the risk (against your identified objectives), managing the risk and then monitoring whether the risk is actually controlled, and whether a further risk treatment needs to be applied.[1]
Risk is the impact of uncertainty on achieving your objectives – the impact can be either positive or negative outcomes (ISO 31000). Governments have multiple objectives they have to meet – health and wellbeing, economic, environmental, ethical and so on. Each of these objectives essentially becomes a risk endpoint. The fundamental tenets of risk assessment are understanding the system (the context), understanding and assessing the risk (against your identified objectives), managing the risk and then monitoring whether the risk is actually controlled, and whether a further risk treatment needs to be applied.[1]
So why are we setting out this risk basis? In the last few days, there has been increasingly conflicting advice from the medical community, COVID risk is increasing at an alarming rate, communication is uncertain, messaging is not meeting its mark, and frustration is running at a concerningly high level.
“Code Red: …..Yesterday morning, an exasperated Premier Gladys Berejiklian threw the switch to her version of Code Red. Off the back of 136 new infections, the highest figure yet, she announced that she had accepted a recommendation from NSW Chief Health Officer Dr Kerry Chant to immediately declare a “national emergency”…..” Deborah Snow, Sydney Morning Herald, 24-25 July 2021, News Review, p25.
“Federation fissures reopen in scrap over Pfizer: On the Australian pandemic scale of drama, confusion and disorderliness it was among the worst…..First, it was NSW premier Gladys Berejiklian blindsiding Canberra, followed by Victoria launching metaphorical grenades across the Murray……Sources familiar with the meeting described it as among the “most tense” national cabinet thus far.” Rob Harris, Sydney Morning Herald, 24-25 July 2021, News, p8.
“ATAGI advice unchanged but youth told to consider jab: …….Allen Cheng, the COVID-19 co-chair of ATAGI, said the balance of risks and benefits was “in a state of flux” in Sydney but noted the group’s role was to provide advice for all of Australia……Australian Medical Association head, Omar Khorshid has told ATAGI: And it may be time for clear advice to all young Australians in Sydney that AZ is a very safe and effective vaccine and it’s the best way to help Sydney get out of a crisis……….ATAGI’s COVID-19 co-chair Christopher Blyth said the group would seek more information, including what other countries were doing, before it finalised its advice.” Katina Curtis, Sydney Morning Herald, 24-25 July 2021, News, p8
Premier set to redirect jabs to boost first doses. States reject NSW bid for more Pfizer vaccines as new cases soar. “…..In what she described as a “national emergency”, [NSW premier] Ms Berejiklian insisted vaccination was the best chance to combat the rising number of cases but Prime Minister, Scott Morrison said hard lockdown in Sydney would be the “key vehicle”.” Alexandra Smith, Lucy Carroll, Lucy Cormack. Sydney Morning Herald, 24-25 July 2021, front page.
“Anti-lockdown protests across Australia as Covid cases surge to record levels in Sydney:… Anti-lockdown protesters have marched in major Australian cities, as Covid cases spiked to record numbers in Sydney and authorities warned of a “continuing and growing problem”….. Similar scenes unfolded in Melbourne and Adelaide, which are both in lockdown, and Brisbane, which is not.” Ben Smee, The Guardian, 24 July 2021.
The impact of uncertainty on achieving many objectives, is increasing. When is an event an incident? When is an incident an emergency? The NSW Premier has declared her own Code Red, but does that have the same meaning across the states, territories and Commonwealth? And what evidence was it based on? There needs to be clarity. One of the first things you get taught in crisis management – is what defines an incident and its level, and what do you do about it. For many in the community, things are moving at such a high velocity that they can’t make decisions on the nature of the situation – incident or not incident, emergency or not emergency. People are struggling with multiple elements of risk. People are frightened, confused and receiving a barrage of information (often of very poor quality and conflicting) from a diversity of sources. Yet people need to make potentially life-changing and life-saving decisions – not just for themselves, but for the overarching benefit of the community. Do I get vaccinated? Which one? What about my family? Do I have to take recommended COVID measures? In the face of this information maelstrom, and analysis paralysis, one of the easiest things to do – is nothing. Doing nothing right now, is really not an option because of the severity of the situation we find ourselves in, the uncertainty on many objectives, is crippling. So how are our governments addressing this issue?
We are both residents of Sydney, living in the escalating COVID crisis, we are both scientists with risk, public health and environmental health backgrounds, and we believe there is a missing piece of the puzzle that is yet to be contemplated – the application of a structured, evidence-based risk framework, for improved decision-making and communication. The framework should allow for:
- Collation of information from multiple contexts including points of entry to Australia, community facilities, sewage surveillance, as well as testing centres.
- Collation of findings from multiple national and international stakeholders.
- Inclusion of input from a range of professionals including, epidemiologists, modellers, community leaders, industry practitioners, local governments, as well as medical practitioners and politicians.
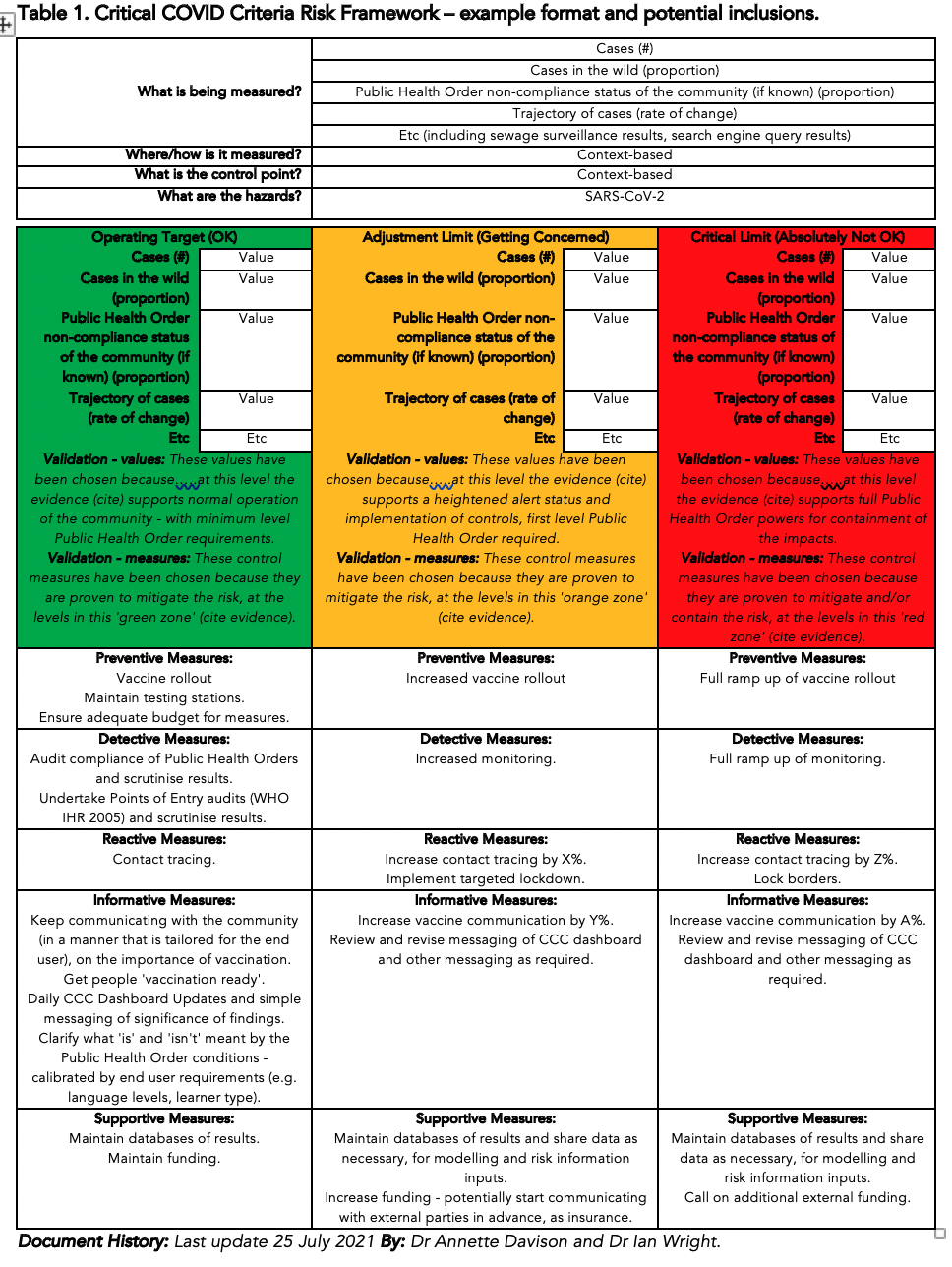
- Identification of parameters and levels (fact-based, not opinion- or belief-based) that can be monitored to help calibrate the risk level.
- Systematized identification of the materiality of the risk – set out within clear boundaries, using simple traffic light visualisation.
- Clear identification of preventive, reactive, detective, supportive and informative risk treatments, for each green, orange and red category of risk.
Setting out such a framework could allow for a transparent, nation-wide approach to risk understanding, communication and decision-making, including daily updated COVID risk dashboards and ‘traffic-lit’ LGAs to communicate risk status, and what that means from a risk management perspective, at the local level. It could also allow for development of a COVID Risk Index by taking into account multiple factors and allowing one index to be applied across the country, as well as potentially, internationally – in a way, a bit like the Southern Oscillation Index for gauging El Niño and La Niña impacts on Australia and the region.
In the water, food and beverage industries, we have been taking this approach for many years – it is called hazard analysis and critical control points – and it can be applied anywhere. We have adapted the thinking and developed a Critical COVID Criteria (CCC) Risk Framework (Table 1). This framework forms a ‘one page’ template which can be added to over time and increased in substance as required – especially as new evidence comes to light (such as the efficacy of lockdowns – type, location, time, strictness; the efficacy of PPE type and the who, when, where of its wearing).
We are at a stage where an evidence-based risk lens is essential if Australia is going to get back on track, deal with the opacity of its decision-making, and reduce the impact of uncertainty on achieving its objectives. Australia’s COVID responses need to be targeted, planned and coordinated as a commonwealth, not reactive, ad hoc and working individually, and this means understanding the risk, managing the risk and monitoring whether the risk is actually being managed, or needs further risk treatment. We know our professionals and politicians are stretched to the limit and under those conditions, it is often difficult to find time to put your head above the ramparts and be strategic. Sometimes all it takes is a new pair of eyes to see a way forward – perhaps our CCC Risk Framework could provide that.
BIO:
Dr Annette Davison is the Australian Water Association’s 2021 Water Professional of the Year for her work on understanding and applying risk in the water industry. She has over 30 years’ experience in the water and environment industries and holds a Higher National Diploma and BSc(Hons) in Applied Biology (majoring in microbiology), a PhD in environmental microbiology and biochemistry, a Master’s degree in Environmental and Local Government Law and is a Graduate of the Australian Institute of Company Directors. Based on assessment of the risk, Annette chose to proceed with an AZ vaccine and has had her first, with the second scheduled.
Dr Ian Wright is water scientist, a science communicator and a senior lecturer in Western Sydney University’s School of Science. He has a Master of Science and PhD and publishes research on a variety of topics including water pollution and environmental health. He works closely with all stakeholders, including local communities, and seeks to manage environmental problems with evidence-based policy. Ian has also received his first AZ vaccination and has booked his second one.
[1] Davison, A. (2020) The Application of ISO 31000 to Drinking Water Quality Risk Management: A Practical Approach. Published by Risk Edge Pty Ltd, Sydney, Australia. ISBN: 978-0-9875560-0-4.