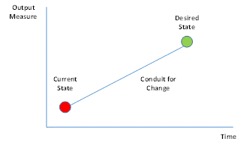
When considering the organizational objectives, we have to know three essential pieces of the puzzle before we can even begin.
When considering the organizational objectives, we have to know three essential pieces of the puzzle before we can even begin.
- What are the measureable objectives?
- What is the baseline?
- What is the relationship to where we need to move the measurable objective?
Assuming the organization can accurately describe the current state in measurable terms, it is important to consider additional attributes.
- Is the measure the correct measure? As an example, are we really measuring nursing costs or are we measuring lost productivity? One is a lagging measure (costs) and one is a leading measure (productivity). Productivity can be dollarized; but which measure is most relevant to the objective?
NO MARGIN – NO MISSION
Even non-for-profits are concerned with “profit” given the phrase “no margin, no mission”, however it may drive the wrong message from a staff perspective. After all, perception is reality. If staff sees the purpose is to save money (Dollar measures), this can be interpreted by staff that leadership is not interested in improving patient care, but rather to save money. As a result leadership may well find staff resentful and have pushback.
Therefore, when leadership is developing strategy objectives, the objective measure should be performance based that reflects effectiveness and efficiencies (quality and speed). These performance measures can easily be translated into costs. Productivity measures, such as, patients per nurse, overtime hours and absenteeism are measurable in unit terms and can be converted into financials. Additionally, staff can see how these objectives directly contribute to patient care, although there still might be caution as change seldom comes without reservations from staff.
Nurse Jones needs, time, knowledge, skill and resources (supplies) to provide quality care to patients. The quality of service is dependent on the Nurses’ competencies and internal supplies or resources (inputs), the processes converts inputs to deliverable (patient care) which results in a bill that eventually gets paid and this can be described as a function of inputs processes and outputs.
Y= f (x): Outputs are a conversion of inputs and if we control and manage inputs we are better at predicting or achieving achieve our outputs / objectives. Thereby, we can monitor and control leading indicators we can better predict outcomes which helps us manage the process to achieve the objectives. In effect, by managing inputs to achieve desired outputs reduces VUCA (Variation, Uncertainty, Complexity & Ambiguity) which reduces enterprise risk.
OUTCOME BASED MISSION
Given the changes in payment models from fee based to outcome based, organizations will have to adjust to make this transition. The challenge is that many organizations are content or “stuck” in the status quo. I say this in general terms meaning “stuck” with using output measures as the primary way to manage organizational performance. However, with some thought and practice it is not hard to consider alternative measures. Any characteristic (Attribute) that can be defined, can be measured and subsequently dollarized. As an example, customer satisfaction is often seen as an enigma, although complaints, time to response for room calls, number of letters of appreciation, referrals, market share, census and of course HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems) are measurable elements of satisfaction which can align with associated costs or revenues.
Focusing on patient centric performance measures is more robust in terms of managing the process than by using dollars. An opportunity to improve patient care, reduce inefficiencies, improve quality, will translate to better satisfaction scores, higher quality better outcomes and less rework and waste. Effectively this is a business opportunity to improve.
The construct of Value = Outcomes / Costs helps to conceptualize moving from fee based to outcome based and helps to put in perspective the value the organization delivers to the community.
- Value in of itself, is a nebulous term. However, if we define value as a function of outcomes and cost, the term itself does not need to be defined further as it will be defined by the nature of the inputs and cost as a ratio. The measurable goal is as outcomes improve, costs go down increasing value, but maintaining cost an increasing outcomes also improves value.
- Outcomes are equivalent to Efficiencies (speed and delivery) and Effectiveness (quality) leading to better patient outcomes.
- Improved outcomes result in shorter lead times, less backlog, fewer rework loops and greater capacity
- Improved effectiveness of the process results in a higher level of quality which is linked to satisfaction internally and externally. As such, improved quality results in better the outcomes of the service (medical) thereby reduces readmissions, secondary infections, etc. which also lowers costs.
- By improving outcomes, we improve the effectiveness and efficiencies while lowering operational costs and improving the value proposition. This leads to a decrease VUCA (Variation, Uncertainty, Complexity and Ambiguity) which reduces organizational risk.
CONCLUSION
In conclusion, when we build our strategy using performance measures we are also building our methodology in how we will reach our objectives. Recall that risk in this case is NOT meeting our objectives as there is a cost associated with failing to achieve these stated goals. By considering the challenge as an opportunity spirits the organization into positive action, not resentment or something else to do, but rather a shared ownership (collaboration) to help the organization seize an opportunity to improve patient outcomes which reduces risk (VUCA) and drives value at the personal, organizational and community level.
Bio:
Steven C. Bradt has 20+ years’ experience working with risk and continuous improvement efforts (Lean, Six Sigma, Leadership, Change, TQM) receiving his primary Continuous Improvement education from Johnson Controls (JCI) Toyota Business Unit (TBU) and Toyota US, UK and Australia and his Six Sigma education from the Six Sigma Academy (Mikel Harry). Steven has supported and worked internationally for Retail. Software, three governments, Office of the Secretary of the Airforce (Chief Management Office), and numerous healthcare organizations in developing sustainable CPI and risk strategy. Steven is currently pursuing his Master of Health Administration Milken Institute School of Public Health at The George Washington University and he was an Honorary Fellow at Manchester Business School.