I recently got a question from one of my clients regarding risks associated with non-compliance in Emergency Department concerning two patient identifiers. The risk identified by my client is not uncommon among many healthcare organizations and falls under operational and compliance risk management. In order to comply with the required organizational practices (ROPs), we first need to have a closer look at it.
I recently got a question from one of my clients regarding risks associated with non-compliance in Emergency Department concerning two patient identifiers. The risk identified by my client is not uncommon among many healthcare organizations and falls under operational and compliance risk management. In order to comply with the required organizational practices (ROPs), we first need to have a closer look at it.
ROPs in this case are the standards that the organization is being held against and must meet. So let us understand what does the ROP actually require? Following is a statement from one of the ROPs that relate to the question at hand. On an average Accreditation Canada had identified that the ROP related to two patient identifier was typically not met in 10% of the cases consistently during 2010-2012.
“Working in partnership with clients and families, at least two person-specific identifiers are used to confirm that clients receive the service or procedure intended for them.”
The Accreditation Canada has some useful guidelines around this. It is the intention of the guideline and this ROP to mitigate several potential risks. These are not limited but could include:
- Privacy breaches
- Allergic reactions
- Discharge of clients to the wrong families
- Medication errors
- Wrong person/procedures.
What can be considered as person-specific identifiers?
These include the client’s full name, home address (when confirmed by the client or family), date of birth, personal identification number, or an accurate photograph ID. It is important to note that the client’s room or bed number, or using a home address without confirming it with the client or family, is not person-specific and should not be used as an identifier.
The situation described above is similar to a scenario where there is a familiarity with the patient. The standard’s guideline speaks to the fact that in a long-term or continuing care where the team member is familiar with the client, one person-specific identifier can be facial recognition. Even in this case it does not negate the fact that one additional unique patient identification needs to be checked before proceeding with patient care.
When checking the client identification most common mistake done is staff members using phrase is “Are you John?” or “Is your date of birth January 1st 1980?”. These are not recommended way of partnering with clients and families when checking for their identification. The staff instead of stating the answer or a positive response, should asking patients for the identifiers (e.g., “What
is your name?” or “What is your date of birth?”).
Working in Emergency Department is stressful and often patients can be in a state where they may or may not be able to respond due to their consciousness. When clients and families are not able to provide the identification information, other sources of identifiers can be explored. These could include wristbands, health records, or government issued identification.
One question that I get asked often is – Is it OK if the two identifiers are taken from the same source. As per Accreditation Canada, it is OK if the two IDs are taken from the same source.
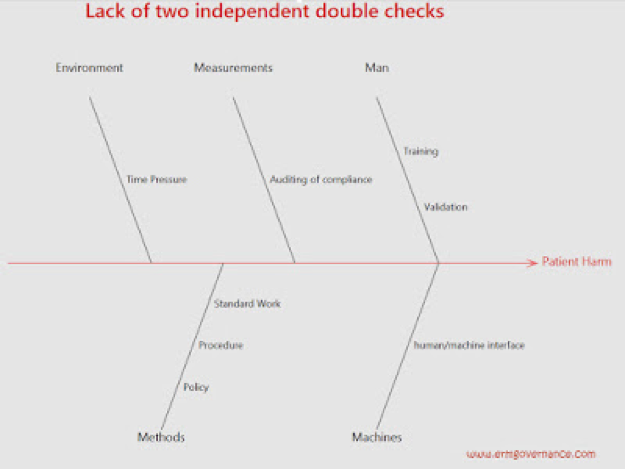
A detailed analysis of this situation can be done through fishbone analysis or five why analysis.
Image Source: www.ERMGovernance.com
Once the team identifies contributing factors affecting their particular environment for the lack of compliance, they can then identify relevant mitigating factors and solutions.
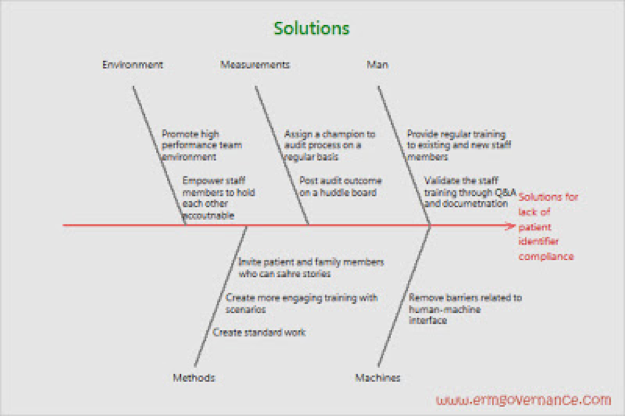
There are many strategies that can be adopted to increase the compliance level. Some of those ideas are presented in the subsequent fishbone titles “Solutions”.
Image Source: www.ERMGovernance.com
Often it is incorrectly believed that having a policy on two identifier is sufficient. Having a policy on two patient identifier is a good starting point. Ultimately, the Unit managers in clinical areas who are responsible for ensuring that the policy is implemented and followed by staff members.
In a situation where a staff are found non-compliant, managers should investigate into reasons for non-compliance and address any potential barriers.
Some key strategies that can be used to monitor and mitigate risk related to patient harm
- Reliable Verification Processes: Organization should create a reliable verification processes that can ensure use of two patient identifiers are being used at the point of care.
- Ensure that the verification process involves use of questions that require an active response.
- Create a high performing team environment by providing education/simulation programs to support the development of teamwork and communication in the emergency department, operating room, or other environments were focused time out is required.
- Coach your care team members on how to give constructive feedback.
- Encourage documentation and reporting of errors involving patient identification. Establish protocols for management of wrong patient incidents including timely notification, documentation, disclosure, and investigation.
- Implement formal strategies to help ensure consistent adherence to patient verification policies/practices. This could include periodic chart audits, analysis of reported incidents, as well as learning from legal claims.
What does the process should look like?
If there are processes related to patient identification then a review of those processes against the accreditation standard as outlined here would be a good starting point. In the absence of a process, a new process or policy related to patient identification verification should be written. At the end of approval of this new policy, it will be crucial to train all staff members as well as introduce a process that can provide ongoing recurring training opportunities for staff.
What should be the content of the new policy?
- It should focus on how to do two independent patient identifier verification.
- It should cover the audit process, frequency and intervals.
- As the team works through this, a process for escalating any barriers related to noncompliance should also be discussed and documented. This would allow an opportunity for broader communication and shared learning around how the issue will be handled and what support may be required from broader team and organizational leaders.
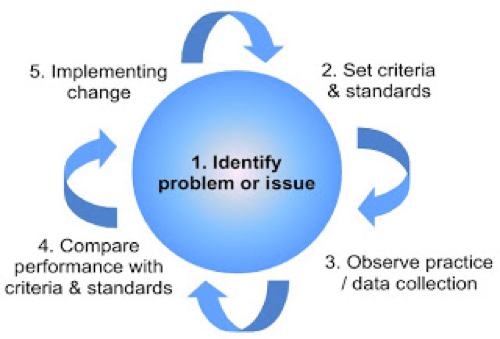
What should the audit process look like?
Image Source: www.wikipedia.org
- Audit process can be simply a list of process flow chart outlining the key steps.
- It should highlight the goal or a problem statement. In this case – to measure if two patient identifier are being used in the emergency department or broadly in the organization at the point of care.
- A criteria / standard should be outlined – in this case, it would include when to do the patient identification verification? (e.g. at the registration, bedside before starting IV etc. etc.)
- A criteria / standard should be outlined regarding- how to do the verification? (e.g. Acceptable vs Unacceptable IDs, Active response vs Passive response).
- Policy / procedure should include information regarding how often an observation / audit will be conducted. The procedure should outline information such as who is responsible for the audit, where the data will be stored and how the data will be used.
- The next step in the process would be to outline what do when standards are not met. How it will be communicated and what will be done to address any identified barriers.
- As the ultimate goal in this case would be to increase compliance, any non-compliance would require implementing a change. What would that PDSA (Plan, Do, Study, Act) look like?
- A policy / procedure should mention training plan, training documentation and retraining frequency.
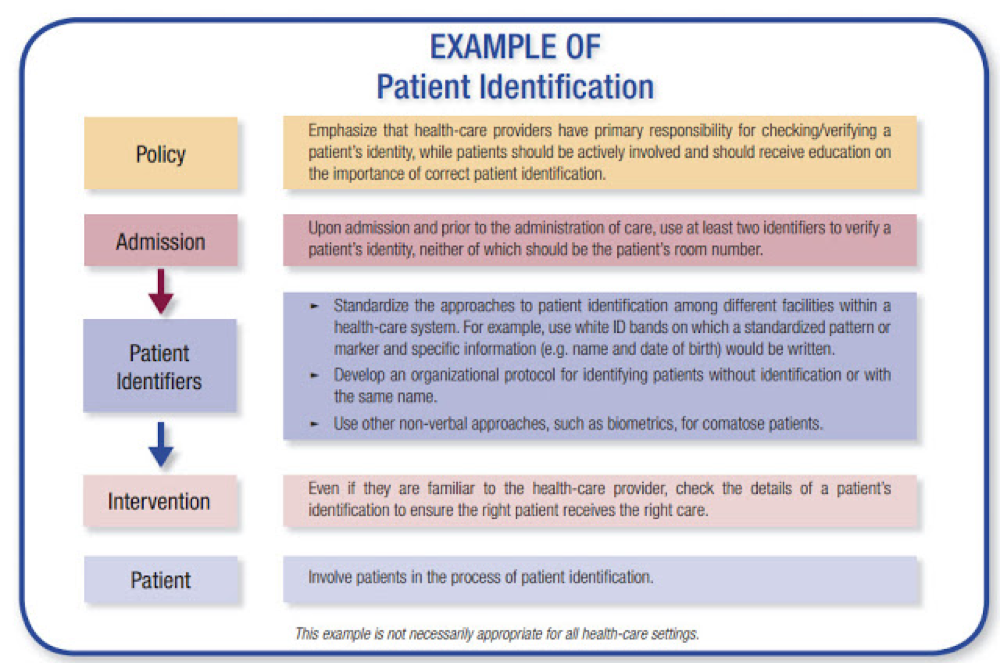
Reference Policy:
http://www.northamptonshire.nhs.uk/resources/uploads/files/PROV_04.pdf
Image Source: http://www.who.int
The identified situation is an example of operational risks that can easily become a reputation and strategic risks in an event a high profile case is surfaced in media potentially tarnishing organization’s reputation and its leaders.
References:
- http://www.northamptonshire.nhs.uk/resources/uploads/files/PROV_04.pdf
- https://www.ncbi.nlm.nih.gov/books/NBK2686/
- https://www.ncbi.nlm.nih.gov/books/NBK2672/pdf/Bookshelf_NBK2672.pdf
- http://vchnews.ca/wp-content/uploads/2015/05/ROP-Fact-Sheet-2015-Two-Identifiers.pdf
- http://www.who.int/patientsafety/solutions/patientsafety/PS-Solution2.pdf
https://accreditation.ca/sites/default/files/char-2013-en.pdf
Bio:
Jignesh is a consultant specialized in managing change involving Lean, Quality Improvement and Healthcare information technology. He has worked for Fortune 500 organizations, public sector as well as led start-ups in healthcare and biotech sector. Jignesh has developed a reputation as a dynamic, innovative, and motivational leader with over 10 years of experience as a champion of quality, safety and risk in diverse organizations. His ability to ask the right questions, and think creatively & strategically gives those he works with a “competitive advantage” in developing winning strategies for their future and the future of their organizations.
Contact: Jignesh.padia@gmail.com
Website: www.ermgovernance.com